The members of the Michigan Shoulder Institute, a division of Orthopaedic Associates of Muskegon, are orthopaedic surgeons who have completed additional training in shoulder reconstruction, including shoulder reconstruction fellowships, sports fellowships, and mini fellowships. They also participate in institute-sponsored, shoulder-specific continuing medical education, submit patient outcomes for quality control, and dedicate significant portions of their practice to shoulder pathology and surgery. They participate in data collection for maximizing patient outcomes and quality monitoring. They also work closely with our partnering hospitals and surgery centers to standardize post-operative care.
Our commitment to optimizing patient outcomes with shoulder disorders has led to the creation of the Michigan Shoulder Institute. It is comprised of orthopaedic surgeons who specialize in non-operative and surgical treatment of all diseases that affect the shoulder. In order to better serve the community, this institute has committed to advancing shoulder surgery outcomes through research, care coordination, and education.
The surgeons of this institute have committed to research through their participation with the American Academy of Orthopaedic Surgeons Shoulder and Elbow Registry, which records and monitors the outcomes of patients with shoulder disorders and how they respond to surgery. Performance analysis allows our surgeons to adjust practice decisions to better serve our patients.
Members of this institute have published numerous peer reviewed articles related to shoulder surgery and have given presentations at national conferences.
Care coordination is achieved by clinical pathways that have standardized pre-operative testing, post-operative medications, and rehabilitation protocols in conjunction with nursing leaders from our affiliate hospitals.
Education is paramount for both patients' understanding and clinician growth. Patient education regarding specific pathology is mandatory for a healthy surgeon-patient relationship and our surgeons participate in community health events. In addition, the surgeons of this group are committed to educating other physicians through journal clubs and lectures. They also help educate future physicians and trainees, with members holding academic affiliations with Michigan State University and Central Michigan University College of Medicine.

Edward JW Shields, MD
Shoulder Reconstruction Specialist
Co-Director, The Michigan Shoulder Institute
For those needing total shoulder replacement, OAM offers a leading-edge, minimally invasive procedure using the Catalyst Stemless Implant that is designed to:
To help educate our patients and prepare them for before, during, and after surgery, we have created an informative video. If you are scheduled for shoulder replacement surgery or are considering it in the future, please click the link below to watch the video.
Frozen shoulder, also called adhesive capsulitis, causes pain and stiffness in the shoulder. Over time, the shoulder becomes very hard to move.
Frozen shoulder occurs in about 2% of the general population. It most commonly affects people between the ages of 40 and 60, and occurs in women more often than men.
Your shoulder is a ball-and-socket joint made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
The head of the upper arm bone fits into a shallow socket in your shoulder blade. Strong connective tissue, called the shoulder capsule, surrounds the joint.
To help your shoulder move more easily, synovial fluid lubricates the shoulder capsule and the joint.
In frozen shoulder, the shoulder capsule thickens and becomes tight. Stiff bands of tissue — called adhesions — develop. In many cases, there is less synovial fluid in the joint.
The hallmark sign of this condition is being unable to move your shoulder - either on your own or with the help of someone else. It develops in three stages:
For additional information about this condition, we have included this complete patient eduction sheet as a pdf to view, download and print:
The rotator cuff is a group of four muscles and their tendons that wrap around to form a "cuff" over the upper end of the arm at the shoulder. The rotator cuff helps guide the shoulder through many motions by allowing lift and rotation to the arm while stabilizing the ball of the shoulder within the socket. The space over the top of the rotator cuff is occupied by a bursa which is a fluid sac between the tendon and the acromion bone. Bursitis, a common condition, is inflammation of this fluid sac and occurs with repetitive overhead activity or overuse of the arm. The term impingement refers to pinching of the rotator cuff tendons and bursa against the acromion bone above it.
A Bankart lesion of the shoulder is a tear of the labrum that causes instability and recurrent dislocations of the shoulder joint. This type of injury often occurs when the shoulder pops out of joint, thereby tearing the labrum. This is quite common in younger patients.
Clavicle fractures occur most frequently after a direct fall on the shoulder. They are especially common in young males. Dirt biking accidents are a frequent mechanism. They present with pain and swelling over the clavicle. In general, greater than 2 cm of shortening or 100% displacement increases the chances of non-union, decreased shoulder strength, decreased endurance, and altered scapular mechanics with pain. Many clavicle fractures can be treated without surgery; however, patients with greater than 2 cm of shortening or greater than 100% displacement typically have better short term outcomes with surgical fixation.
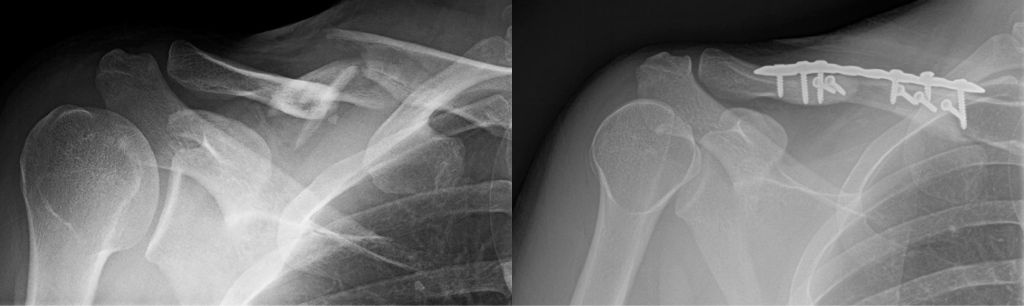
Clavicle radiographs demonstrating a multi-fragmented right clavicle fracture (left image), treated with open reduction and internal fixation (right image)
Distal clavicle or "AC" (acromioclavicular) arthritis results in pain over the shoulder, especially right on top of the shoulder with overhead and cross body maneuvers. Sometimes pain from AC arthritis can be present in addition to rotator cuff pain or a completely separate issue. Pain from the AC joint is usually quite distinct from rotator cuff pain but they can be confused. Arthritis of the AC joint is initially treated with physical therapy, NSAIDs, and cortisone injections. When these measures fail to help, a limited distal clavicle resection surgery can be performed to open up the space between the clavicle and acromion. This can be performed arthroscopically and requires only a few days of immobilization afterwards.
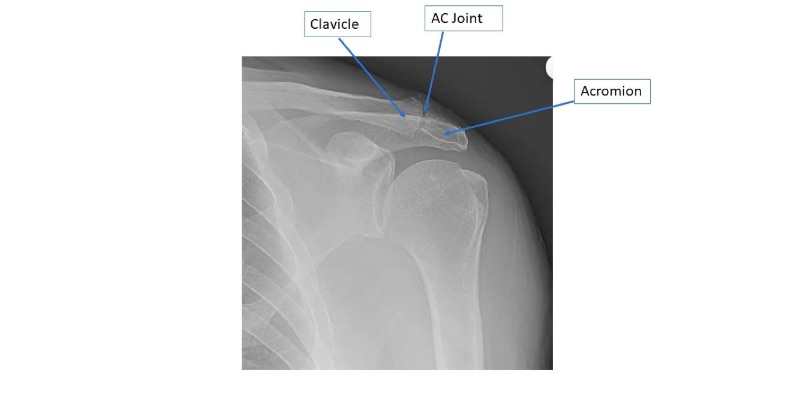
Shoulder radiographs demonstrating "AC" arthritis.
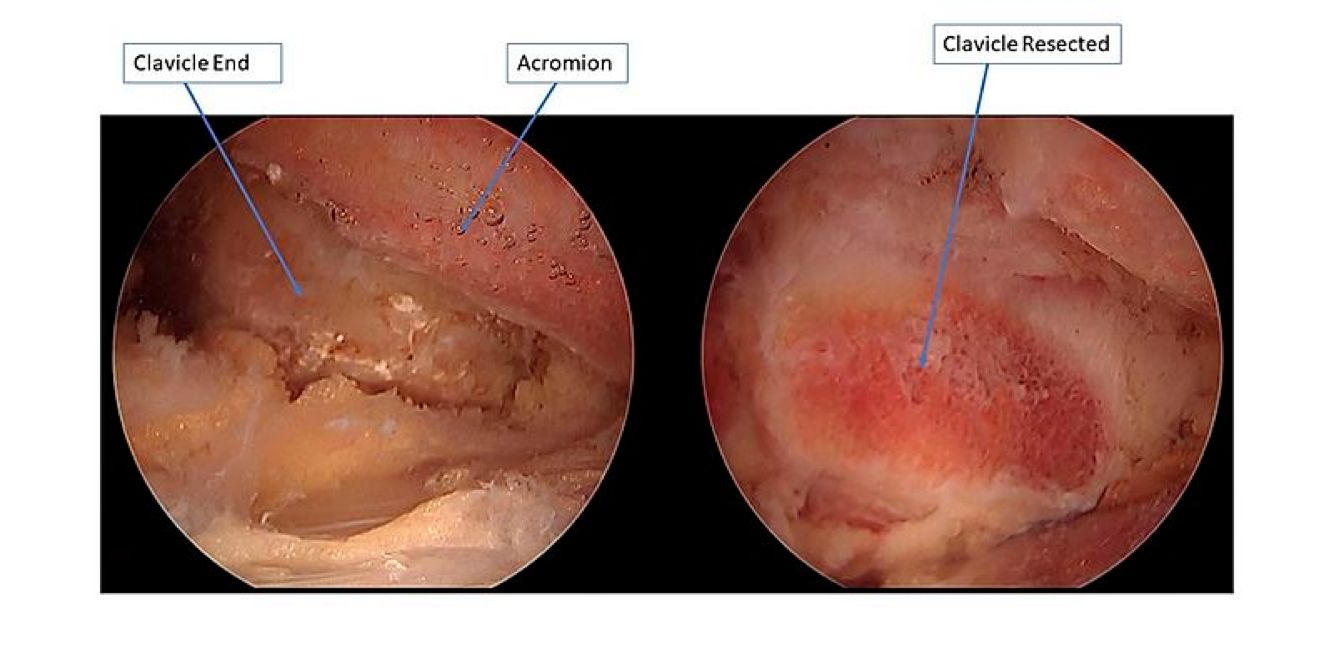
Arthroscopic images before and after distal clavicle resection, demonstrating an increased space between the distal arthritic clavicle and the acromion.
Similar to the hip, the shoulder joint is a ball-and-socket joint. The ball of the upper arm bone is held in place within the socket of the shoulder blade. However, the shoulder socket itself is extremely shallow and unstable. The bones of the shoulder are not held in place adequately, thereby requiring extra support. To help compensate for this instability, the shoulder joint has a cuff of cartilage (labrum) that forms a cup for the end of the arm bone to move within. The labrum wraps around the shallow shoulder socket, thus making the socket deeper. In addition, the bicep muscle tendons of the upper arm attach to the shoulder just above the labrum. This arrangement makes the shoulder much more stable and allows for a very wide range of movements.
A shoulder or arm injury may cause a labrum tear, but the labrum itself may simply become brittle with age and may fray and tear as part of the aging process.
Proximal humerus fractures can involve four sections of the proximal humerus – the shaft, the ball, the lesser tuberosity, and greater tuberosity. Treatment options include non-operative treatment, surgical fixation, and replacement. The vast majority can be successfully treated without surgery. Depending on age, fragment displacement and angulation, some patients have better outcomes with surgical repair or replacement.

Shoulder radiographs demonstrating a complex proximal humerus fracture on the left, treated with a reverse shoulder arthroplasty on the right.
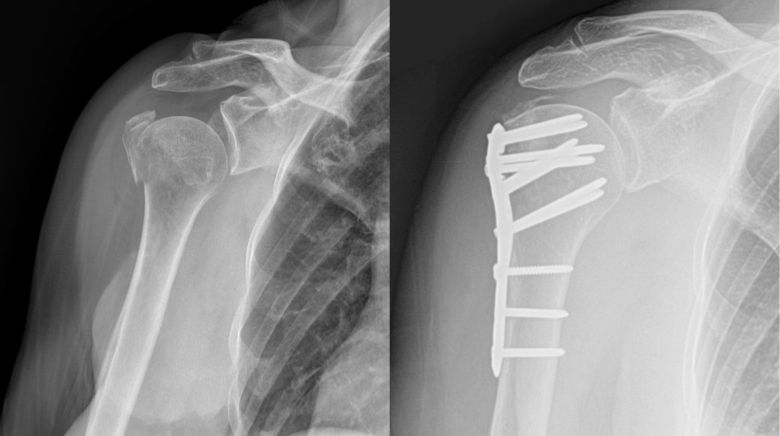
Shoulder radiographs demonstrating a valgus impacted proximal humerus fracture (left image), treated with open reduction internal fixation (right image).
A rotator cuff tear is a common cause of pain and disability among adults. Each year, over a million people in the United States go to their doctors because of a rotator cuff problem. A torn rotator cuff will weaken your shoulder. This means that many daily activities, like combing your hair or getting dressed may become painful and difficult to do.
Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle). The shoulder is a ball-and-socket joint: The ball, or head, of your upper arm bone fits into a shallow socket in your shoulder blade.
Your arm is kept in your shoulder socket by your rotator cuff. The rotator cuff is a network of four muscles that come together as tendons to form a covering around the head of the humerus. The rotator cuff attaches the humerus to the shoulder blade and helps to lift and rotate your arm.
There is a lubricating sac called a bursa between the rotator cuff and the bone on top of your shoulder (acromion). The bursa allows the rotator cuff tendons to glide freely when you move your arm. When the rotator cuff tendons are injured or damaged, this bursa can also become inflamed and painful.
When one or more of the rotator cuff tendons is torn, the tendon no longer fully attaches to the head of the humerus. Most tears occur in the supraspinatus tendon, but other parts of the rotator cuff may also be involved. In many cases, torn tendons begin by fraying. As the damage progresses, the tendon can completely tear, sometimes with lifting a heavy object.
There are different types of tears:
For additional information about this condition, we have included this complete patient eduction sheet as a pdf to view, download and print:
Shoulder dislocations can be partial, with the ball of the upper arm coming just partially out of the socket. This is called a subluxation. A complete dislocation means the ball comes all the way out of the socket.
Once the ligaments, tendons, and muscles around the shoulder become loose or torn, dislocations can occur repeatedly. Chronic shoulder instability is the persistent inability of these tissues to keep the arm centered in the shoulder socket.
Severe injury, or trauma, is often the cause of an initial shoulder dislocation. When the head of the humerus dislocates, the socket bone (glenoid) and the ligaments in the front of the shoulder are often injured. The torn ligament in the front of the shoulder is commonly called a Bankart lesion. A severe first dislocation can lead to continued dislocations, giving out, or a feeling of instability.
For additional information about this condition, we have included this complete patient eduction sheet as a pdf to view, download and print:
One of the most common physical complaints is shoulder pain. Your shoulder is made up of several joints combined with tendons and muscles that allow a great range of motion in your arm. Because so many different structures make up the shoulder, it is vulnerable to many different problems. The rotator cuff is a frequent source of pain in the shoulder.
Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
Your arm is kept in your shoulder socket by your rotator cuff. These muscles and tendons form a covering around the head of your upper arm bone and attach it to your shoulder blade.
There is a lubricating sac called a bursa between the rotator cuff and the bone on top of your shoulder (acromion). The bursa allows the rotator cuff tendons to glide freely when you move your arm.
Rotator cuff pain commonly causes local swelling and tenderness in the front or side of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position. You may have sudden pain with lifting and reaching movements.
For additional information about this condition, we have included this complete patient eduction sheet as a pdf to view, download and print:
A direct fall on the shoulder can cause a "shoulder separation" or acromioclavicular (AC) joint sprain. This injury is usually sports related. Some separations happen in car accidents or falls. This is not the same as a shoulder dislocation, which occurs at the large joint where the arm attaches to the shoulder, although the two may appear to be the same.
The shoulder separation, or acromioclavicular (AC) dislocation, is an injury to the junction between the collarbone and the shoulder. It is usually a soft-tissue or ligament injury but may include a fracture (broken bone).
High grade sprains can result in elevation of the distal end of the clavicle resulting in a bump or prominence. These are usually treated without surgery. If significant displacement or pain persists after non-operative treatment, surgical repair can be performed. Acute injuries can be treated with plating or other fixation methods, whereas chronic tears require ligament reconstruction.

Shoulder radiographs demonstrating a "shoulder separation" or acromioclavicular sprain ("AC sprain"), with the clavicle end elevated away from the acromion (left image), and repair with open reduction internal fixation (right image).
The sternoclavicular (SC) joint is the pivot on which the shoulder girdle moves on the trunk. It is located at the junction of the collar bone and the breast bone. Dislocation of this joint most often results from a fall onto the shoulder.
The type of treatment your physician prescribes will depend entirely on the type of injury to your joint.
Anterior or forward dislocations are the most common and can sometimes occur with minimal trauma in patients with generalized looseness in their joints. Posterior dislocation of the sternoclavicular joint is less common than the anterior type but is potentially much more serious. Damage to important structures located behind the sternoclavicular joint (arteries, veins, nerves, esophagus, trachea) can cause difficulty breathing and swallowing, poor circulation to the arm and hand, and nerve damage.
The labrum is a fibrous bumper that helps to stabilize the shoulder joint. It provides an attachment site for a variety of other shoulder structures including the capsule, ligaments and biceps tendon. When the superior labrum is detached or torn at the site of the biceps tendon insertion, it is termed a superior labrum anterior to posterior tear (SLAP). A variety of injuries may cause damage to the superior part of the labrum where the biceps tendon inserts. The most common type of injuries are repetitive over arm motion such as throwing a ball, falling on an outstretched arm or lifting a heavy object.
Overhead athletes or patients involved in repetitive overhead work can damage the superior labrum. This often generates a deep or posterior pain in the shoulder joint accompanied by a clicking, catching or popping sensation. There may be weakness with overhead activity. The throwing athlete often notices diminished velocity and control with throwing a ball. A thorough evaluation by your sports medicine physician is most appropriate to confirm this diagnosis. X-rays may be obtained in order to rule out any type of bony damage. An MRI may also be obtained in order to determine the degree of superior labral injury, as well as the existence of any injury in the adjacent capsule, ligaments or biceps tendon.
View the physical therapy videos to learn about necessary exercises for before and after surgical treatments..
Our practice collects patient outcomes for all shoulder surgery in an effort to improve outcomes. In addition, our surgeons have published numerous scientific articles and given dozens of scientific presentations locally and nationally focused on shoulder and elbow disease and treatment.
Shields E, Kouetier D, Wiater JM. Rate of Improvement in Outcome Measures after Reverse Total Shoulder Arthroplasty: A Longitudinal Study with Two-Year Follow-Up. Journal of Shoulder and Elbow Arthroplasty, 2019; July(3): 1-7. https://doi.org/10.1177/2471549219861446
Raap C, Shields E, Wiater JM. Venousthromboembolus in Shoulder Surgery. JAAOS, 2018; Apr 15;27(8):265-274. doi: 10.5435/JAAOS-D-17-00763. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/30480588
Simha S, Shields E, Wiater JM. Periprosthetic Infections of the Shoulder. JBJS Reviews, 2018; Sept 6(9): e6 DOI: 10.2106/JBJS.RVW.17.00191 Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/30234597
Thorsness R, Iannuzzi J, Shields E, Noyes K, Voloshin I. The Cost-Effectiveness of Open Reduction and Internal Fixation Compared with Hemiarthroplasty in the Management of Complex Proximal Humerus Fractures. Journal of Shoulder and Elbow Arthroplasty, 2018; Jan 2:1-9. https://doi.org/10.1177/2471549217751453
Shields E, Thirukumaran C, Thorsness R, Noyes K, and Voloshin I. Patient Factors Influencing Return to Work and Cumulative Financial Claims After Rotator Cuff repair in Geriatric Workers Compensation Cases. Geriatric Orthopaedic Surgery and Rehabilitation, 2017; Dec 8(4): 208-214. doi: 10.1177/2151458517732209 Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/29318082
Shields E and Wiater JM. Patient Outcomes after Revision of Anatomic Total Shoulder Arthroplasty to Reverse Shoulder Arthroplasty for Rotator Cuff Failure or Component Loosening: A Matched Cohort Study. JAAOS, 2017; Feb 15;27(4):e193-e198. doi: 10.5435/JAAOS-D-17-00350 Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/30216243
Shields E, Koueiter D, Maerz T, Schwark A, Wiater JM. Previous Rotator Cuff Repair is Associated with Inferior Clinical Outcomes after Reverse Total Shoulder Arthroplasty. Orthopaedic Journal of Sports Medicine, 2017; Oct; 5(10): doi: 10.1177/2325967117730311 Pubmed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5637974/
Shields E, Ho A, and Wiater JM. Subscapularis Tendon Management During Anatomic and Reverse Total Shoulder Arthroplasty. Minerva Ortopedica E Traumatologica, 2017; September;68(3):168-78. Link: https://www.minervamedica.it/en/journals/minerva-ortopedica-traumatol/article.php?cod=R14Y2017N03A0168
Thorsness R, Shields E, Owens K, Gorczyca J, Voloshin I. Open Reduction and Internal Fixation Versus Hemiarthroplasty in the Management of Complex Articular Fractures and Fracture-dislocations of the Proximal Humerus. Journal of Shoulder and Elbow Arthroplasty, 2017; June;1:1-7. Link: https://doi.org/10.1177/2471549217709364
Shields E, Ho A, and Wiater JM. Management of the Subscapularis Tendon During Total Shoulder Arthroplasty. Journal of Shoulder and Elbow Surgery, 2017; Apr;26(4):723-731. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/28111182
Shields E, Thirukumaran C, Thorsness R, Noyes K, and Voloshin I. Patient Factors Influencing Return to Work and Cumulative Financial Claims After Clavicle Fractures in Workers Compensation Cases. Journal of Shoulder and Elbow Surgery,2016;25(7):1115-21. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/27066964
Thorsness R, Shields E, Iannuzzi J, Zang L, Noyes K, Voloshin I. Cost Drivers after Surgical Management of Proximal Humerus Fractures in Medicare Patients. Journal of Orthopaedic Trauma, 2016;30(5):262-8. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/26670287
Shields E, Sundem L, Childs S, Maceroli M,; Humphrey C, Ketz JP,Gorczyca JT. The Impact of Residual Angulation on Patient Reported Functional Outcome Scores after Non-operative Treatment for Humeral Shaft Fractures. Injury, 2016;47(4):914-8. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/26754807
Shields E, Behrend C, Beiswenger T, Strong B, English E, Maloney M, Voloshin I. Scapular Dyskinesis Following Displaced Fractures of the Middle Clavicle. Journal of Shoulder and Elbow Surgery, 2015;24(12):e331-6. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/26169903
Shields E, Sundem L, Childs S, Maceroli M, Humphrey C, Ketz J, and Gorczyca J. Factors Predicting Patient Reported Functional Outcomes following Humeral Shaft Fractures. Injury, 2015;46(4): 693-8. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25697858
Shields E, Olsen J, Miller R, Rouse L, Maloney M, Voloshin I. A Comparison of a Single Incision Technique using Cortical Button with Interference Screw versus a Double Incision Technique using Suture Fixation through Bone Tunnels for Distal Biceps Brachii Tendon Repairs. American Journal of Sports Medicine, 2015;43(5):1072-6. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25700163
Shields E, Thirukumaran C, Thorsness R, Noyes K, Voloshin I. An Analysis of Adult Patient Risk Factors and Complications within 30 days after Arthroscopic Shoulder Surgery. Arthroscopy, 2015;31(5):807-15. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25661861
Shields E, Iannuzzi J, Thorsness R, Noyes K, and Voloshin I. Post-operative Morbidity by Procedure and Patient Factors Influencing Major Complications within 30 Days Following Shoulder Surgery. Orthopaedic Journal of Sports Medicine. 2014;2(10). Electronic Publication. DOI: 10.1177/2325967114553164 Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/26535274
Chen C, Behrend C, Shields E, English C; Maloney M, Voloshin I. Effects of Debridement of Biceps Tendon Insertion and Superior Labrum on Stability of the Shoulder Joint in Cadaveric Concavity-Compression Model. Arthroscopy, 2014;30(12):1557-61. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25129863
Shields E, Mirabelli M, Amsdell S, Thorsness R, Goldblatt J, Maloney M, and Voloshin I. Functional and Ultrasonography Imaging Outcomes of Arthroscopic Simultaneous Rotator Cuff and Bankart Repair after Shoulder Dislocation. American Journal of Sports Medicine. 2014;42(11):2614-20. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25261085
Olsen J, Shields E, Miller R, Maloney M, Voloshin I. A Comparison of the Tension Slide with Interference Screw versus Suture Anchor Techniques for Distal Biceps Tendon Repairs. Journal of Shoulder and Elbow Surgery. 2014;23(11):1607-11. Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25219472
Shields E, Iannuzzi J, Thorsness R, Noyes K, Voloshin I. Peri-Operative Complications Following Hemi- and Total Shoulder Arthroplasty are Equivalent. Journal of Shoulder and Elbow Surgery. 2014;23(10):1449-53. DOI: 10.1016/j.jse.2014.01.052 Pubmed: https://www.ncbi.nlm.nih.gov/pubmed/25219472
AAOS Annual Meeting, March 2020, Orlando, FL-Meeting Canceled Rate of Improvement in Outcomes Measures after Reverse Total Shoulder Arthroplasty: A Longitudinal Study with Two-Year Follow-Up Authors: Shields, E; Koueiter, D; Wiater, JM
ASES Annual Closed Meeting, October 2017, New Orleans, LA Previous Rotator Cuff Repair is Associated with Inferior Clinical Outcomes After Reverse Total Shoulder Arthroplasty Authors: Shields, E; Koueiter, D; Maerz, T; Schwark, A; Wiater, JM
The 13th International Congress of Shoulder and Elbow Surgery, May 2016, Jeju, Korea Open Reduction And Internal Fixation Versus Hemiarthroplasty In The Management Of Complex Articular Fractures And Fracture-Dislocations Of The Proximal Humerus Authors: Thorsness, R; Shields, E; Owens, C; Gorczyca, J; Voloshin, I
American Shoulder and Elbow Society, Closed Meeting October 2015, Ashville, NC Patient Factors Influencing Return To Work And Cumulative Financial Claims After Clavicle Fractures In Workers Compensation Cases. Authors: Shields, E; Thirukumaran, C; Thorsness, R; Noyes, K; Voloshin, I
Orthopaedic Trauma Association, National Meeting, October 2015, San Diego, CA The Impact of Residual Angulation on Patient Reported Functional Outcome Scores after Non-operative Treatment for Humeral Shaft Fractures. Authors: Shields, E; Sundem, L; Childs, S; Maceroli, M; Humphrey, C; Ketz, J; Soles, G; Gorczyca, J
Orthopaedic Trauma Association, National Meeting, October 2015, San Diego, CA Scapular Dyskinesis Following Displaced Fractures of the Middle Clavicle. Authors: Shields, E; Behrend, C; Beiswenger, T; Strong, B; Maloney, M; Voloshin, I
European Society for Surgery of the Shoulder and Elbow, September 2015, Milano, Italy Scapular Dyskinesis Following Displaced Fractures of the Middle Clavicle. Authors: Shields, E; Behrend, C; Beiswenger, T; Strong, B; Maloney, M; Voloshin, I
American Shoulder and Elbow Society, Specialty Day Meeting, March 2015, Las Vegas, NV The Cost-Effectiveness Of Open Reduction And Internal Fixation Compared With Hemiarthroplasty In The Management Of Complex Proximal Humerus Fractures. Authors: Thorsness, R; Iannuzzi, J; Shields, E; Noyes, K; Voloshin, I
American Orthopaedic Association/COA combined meeting June 2014, Montreal, Canada The cost-effectiveness of open reduction and internal fixation compared with hemiarthroplasty in the management of complex proximal humerus fractures. Authors: Thorsness, R; Iannuzzi, J; Shields, E; Noyes, K; Voloshin, I
Arthroscopy Association of North America, Annual Meeting May 2014, Hollywood, FL Defining High Risk Shoulder Procedures: An analysis of the National Surgical Quality Improvement Database Authors: Shields, E; Iannuzzi, J; Thorsness, R; Noyes, K; Voloshin, I
Arthroscopy Association of North America, Annual Meeting May 2014, Hollywood, FL Functional and Ultrasonography Imaging Outcomes of Arthroscopic Simultaneous Rotator Cuff and Bankart Repair after Shoulder Dislocation Authors: Shields, E; Mirabeli, M; Amsdell, S; Thorsness, R; Goldblatt, J; Maloney, M; Voloshin, I
American Academy of Orthopaedic Surgeons, March 2014, New Orleans, LA Open Reduction and Internal Fixation versus Hemiarthroplasty In The Management Of Proximal Humerus Fractures Authors: Thorsness, R.; Shields, E.; Iannuzzi, J; Zhang, L; Noyes, K; Voloshin, I.
Orthopaedic Trauma Association, National Meeting, October 2013, Phoenix, AZ Functional Outcome Scores of Humeral Shaft Fractures in Patients Treated Non-operatively Compared to Those Treated Surgically Authors: Shields, E; Maceroli, M; Sundem, L; Childs, S; Hadiono, A; Humphrey, C; Gross, J; Ketz, J; Gorczyca, J
American Shoulder and Elbow Society, Closed Meeting October 2013, Las Vegas, NV Functional and Ultrasonography Imaging Outcomes of Arthroscopic Simultaneous Rotator Cuff and Bankart Repair after Shoulder Dislocation Authors: Shields, E; Mirabeli, M; Amsdell, S; Thorsness, R; Goldblatt, J; Maloney, M; Voloshin, I
Beaumont Health Resident and Fellow Research Forum, May, 2017, Royal Oak, MI The Effect of Previous Rotator Cuff Repair on Clinical Outcomes after Reverse Total Shoulder Arthroplasty Authors: Shields E, Koueiter D, Maerz T, Schwark A, Wiater JM
American Orthopaedic Association, Annual Meeting, June 2016, Seattle, WA Patient Factors Influencing Return to Work and Cumulative Financial Claims After Rotator Cuff Repair in Workers Compensation Cases Authors: Shields, E; Thirukumaran, C; Thorsness, R; Noyes, K; Nicandri, G; Voloshin, I
The 13th International Congress of Shoulder and Elbow Surgery, May 2016, Jeju, Korea Scapular Dyskinesis Following Displaced Fractures of the Middle Clavicle. Authors: Shields, E; Behrend, C; Beiswenger, T; Strong, B; Maloney, M; Voloshin, I
American Shoulder and Elbow Society, Closed Meeting October 2015, Ashville, NC Open Reduction And Internal Fixation Versus Hemiarthroplasty In The Management Of Complex Articular Fractures And Fracture-Dislocations Of The Proximal Humerus Authors: Thorsness, R; Shields, E; Owens, C; Gorczyca, J; Voloshin, I
American Orthopaedic Association, Annual Meeting, June 2015, Providence, RI Open Reduction and Internal Fixation versus Hemiarthroplasty in the Management of Complex Articular Fractures and Fracture-Dislocations of the Proximal Humerus Authors: Thorsness, R; Shields, E; Owens, K; Gorczyca, J; Voloshin, I
Orthopaedic Trauma Association, Annual Meeting, October 2014, Tampa Bay, FL Factors Predicting Satisfactory Functional Outcomes in Patients Following Humeral Shaft Fractures Authors: Shields, E; Sundem, L; Childs, S; Maceroli, M; Soles, G; Humphrey, C; Ketz, J; Gorczyca, J
American Orthopaedic Association/COA Combined Meeting, June 2014, Montreal, Canada Functional and Ultrasonography Imaging Outcomes of Arthroscopic Simultaneous Rotator Cuff and Bankart Repair after Shoulder Dislocation Authors: Shields, E; Mirabeli, M; Amsdell, S; Thorsness, R; Goldblatt, J; Maloney, M; Voloshin, I
American Shoulder and Elbow Society, Closed Meeting, October 2013, Las Vegas, NV Open Reduction and Internal Fixation versus Hemiarthroplasty In The Management Of Complex Articular Fractures And Fracture-Dislocations Of The Proximal Humerus Authors: Thorsness, R; Shields, E; Owens, K; Voloshin, I
American Orthopaedic Association Annual Meeting, June 2013, Denver, CO Scapula Dyskinesis Following Treatment of Displaced Fractures of the Midshaft Clavicle Authors: Behrend, C., Shields, E; English, C; Beiwenger, T; Maloney, M.D., Voloshin, I.
International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine Annual Meeting, May 2013, Toronto, Canada Scapular Dyskinesis Following Displaced Fractures of the Midshaft Clavicle Authors: Behrend, C; Beiswenger, T; English, C; Shields, E; Maloney, M; Voloshin, I
Arthroscopy Association of North America Annual Meeting, April 2013, San Antonio, TX Scapular Dyskinesis Following Displaced Fractures of the Midshaft Clavicle Authors: Behrend, C; Beiswenger, T; English, C; Shields, E; Maloney, M; Voloshin, I
Arthroscopy Association of North America Annual Meeting, April 2013, San Antonio, TX Effects of Debridement of Biceps Tendon Insertion and Superior Labrum on Stability of the Shoulder Joint in Cadaveric Concavity-Compression Model Authors: Chen, C., Behrend, C., Shields, E; English, C; Maloney, M.D., Voloshin, I.
Injuries can happen anytime so we have immediate appointments available at our Muskegon and Grand Haven offices. Our orthopaedic urgent care is open to accommodate same day visits for the evaluation of shoulder injuries.